Abstract
Introduction: Neutrophil-Lymphocyte ratio is prognostic in solid tumors and lymphomas which may serve as an index of anti-tumor immune response. The role of immune surveillance in myeloproliferative neoplasms (MPNs) is being increasingly explored. In this study, we aimed to investigate whether such surrogate markers of immune response offers prognostic significance in MPNs. Myelofibrosis (MF) is characterized by leukoerythoblastosis in the peripheral blood which leads to relative lymphopenia. To account for this, we modified the neutrophil:lymphocyte ratio by instead assessing the prognostic significance of relative lymphocytosis in terms of the total white blood cell (WBC):lymphocyte ratio (WLR). Further, given recent evidence of enhanced immunogenicity of CALR mutant MPN cells, we explored if WLR varies based upon driver mutation.
Methods: We retrospectively reviewed MF patients seen at our institution between 1/1/2001 and 5/1/2017. MF was defined by 2016 WHO criteria. Laboratory values were calculated at first presentation and overall survival (OS) was calculated from time of first presentation. WLR defined as WBC/absolute lymphocyte count (ALC). A WLR cutpoint of 7 was based on median WLR value.
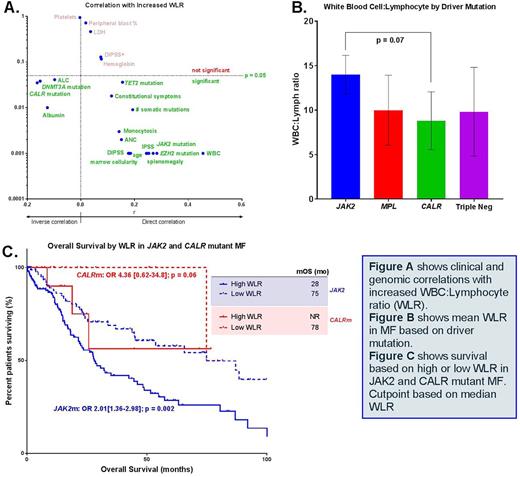
Results: Of 436 total MF patients, 431 had baseline lab values at time of first presentation, and 319 were informative for somatic gene mutations. Two-hundred forty-nine (78%) were JAK2 mut, 36 (11%) were CALR mut, 17 (5%) were MPL mut and 17 (5%) were triple-negative. On univariate analysis, absolute lymphocyte count (ALC) did not correlate with OS (p = 0.82), and there was no difference in ALC based on driver mutation. WBC:ALC ratio (WLR), however, was associated with inferior OS (p = 0.001) in univariate analysis. High WLR directly correlated with age (p < 0.001), monocytosis (p < 0.001), increased peripheral blasts (p < 0.001), immature myeloid cells (p < 0.001), bone marrow cellularity (p < 0.001), splenomegaly (p = 0.001), constitutional symptoms (p = 0.02), IPSS (p < 0.001) and DIPSS prognostic scores (p =0.01), mutations in JAK2 (p < 0.001), TET2 (p = 0.04) and EZH2 (p < 0.001) and total number of somatic mutations (p = 0.009). Low WLR correlated with presence of CALR (p = 0.04) and DNMT3A mutations (p = 0.04). On multivariate analysis, controlling for DIPSS, albumin, and bone marrow fibrosis, WLR remained a significant prognostic co-variate (p = 0.04).
Comparison of WLR according to specific driver mutation showed a trend toward lower WLR in CALR mutant versus JAK2 mutant MF (p =0.07). Low WLR was also associated with improved OS (HR 0.67 [0.51-0.89]; p = 0.005) in the entire MF cohort as well as in JAK2 mut (p = 0.002) and CALR mut subgroups (p = 0.06).
Lastly, we assessed the relationship between WLR and variable allele frequency (VAF) of JAK2 and CALR driver mutations as well as the commonly occurring somatic mutations ASXL1 (n = 53) and SRSF2 (n = 29). High WLR was directly associated with VAF of JAK2 (p = 0.01) and CALR (p = 0.04), though the correlation was stronger with CALR than JAK2 (r2 = 0.30 vs 0.05). A trend towards a positive correlation was found between WLR and ASXL1 VAF (p = 0.07) whereas there was no correlation with SRSF2 VAF (p = 0.70).
Conclusion: WLR is an independent prognostic co-variate in patients with MF with higher ratios conferring inferior outcomes. Decreased WLR in CALR mut compared with JAK2mut MF patients coupled with the strong correlation with CALR VAF suggests this may underlie the more favorable prognosis in CALR mut patients. Further investigations are warranted to discern the biological responses driving the changes in WLR index.
Epling-Burnette: Incyte: Research Funding; Forma Therapeutics: Research Funding; Celgene: Research Funding. Padron: Incyte: Honoraria, Research Funding. Sallman: Celgene: Research Funding. Lancet: Pfizer: Other: Institutional research funding; Biopath, Biosight, Boehringer Ingelheim, Celator/Jazz, Celgene, Janssen, Karyopharm Therapeutics, and Novartis: Consultancy. Komrokji: Novartis: Honoraria, Speakers Bureau; Celgene: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal